Researchers' Zone:
A Sweet Breakthrough in Prostate Cancer Screening
Early results show promise for a new test that targets sugar patterns in prostate tissue.
If you're a man and live in Denmark, prostate cancer is the most common malignancy you’re likely to develop. About 1 in 11 will be diagnosed with prostate cancer at some point in their lives.
Prostate cancer is very treatable if caught early, when the disease has not yet spread beyond the prostate gland, and even in the case of cancer moved to other parts of the body, such as in the case of metastatic cancer with the worse prognosis, it is more treatable when quickly diagnosed.
Great! – if only we were actually good at catching the disease early.
Around 2900 people died from prostate cancer in Denmark in 2023, which is the highest number in a decade. Imagine if we could reduce that number simply by improving our screening for the disease.
Our research group at Aarhus University and Aarhus University Hospital has been working on a new method to test for prostate cancer, based on the sugarcoating properties of proteins produced by prostate - and now it looks like we have succeeded.
The results have been published in Analytical Chemistry.
Current test has major flaws
As many other cancers, prostate cancer is tricky to detect early —it often develops silently, without any noticeable symptoms in its early stages.
Right now, the most common way to screen for it in wide population is a simple blood test that measures levels of a protein called PSA (prostate-specific antigen).
PSA is made by prostate cells and plays a role in semen production. Some of it naturally enters the bloodstream, and in healthy men, PSA levels are usually below 4.9 ng/mL.
But in men with prostate cancer, these levels can rise dramatically, sometimes exceeding 20 ng/mL.
The U.S. Food and Drug Administration (FDA) approved PSA testing as a prostate cancer screening tool back in 1996, but since then, researchers have discovered that the test has major flaws:
It isn’t always reliable and can lead to both false alarms and missed diagnoses (read more about this in the box below).
Furthermore, if the PSA blood tests are positive, further tests such as MRI and tissue biopsy are conducted, but they are either painful (and can still miss the tumor) or expensive and time consuming, and therefore impractical for frequent screening.
Therefore, a simple blood test that could actually determine if you have prostate cancer without further tests would be far easier for both early detection and ongoing monitoring.
Due to these flaws in PSA testing, the U.S. Preventive Services Task Force (USPSTF) even recommended against routine PSA screening in 2012. Despite this, PSA tests remain widely used, while scientists continue searching for better, more accurate ways to detect prostate cancer early.
A Sugar-Coated Clue
Therefore, we have focused on an overlooked aspect of the PSA protein: its sugar coating.
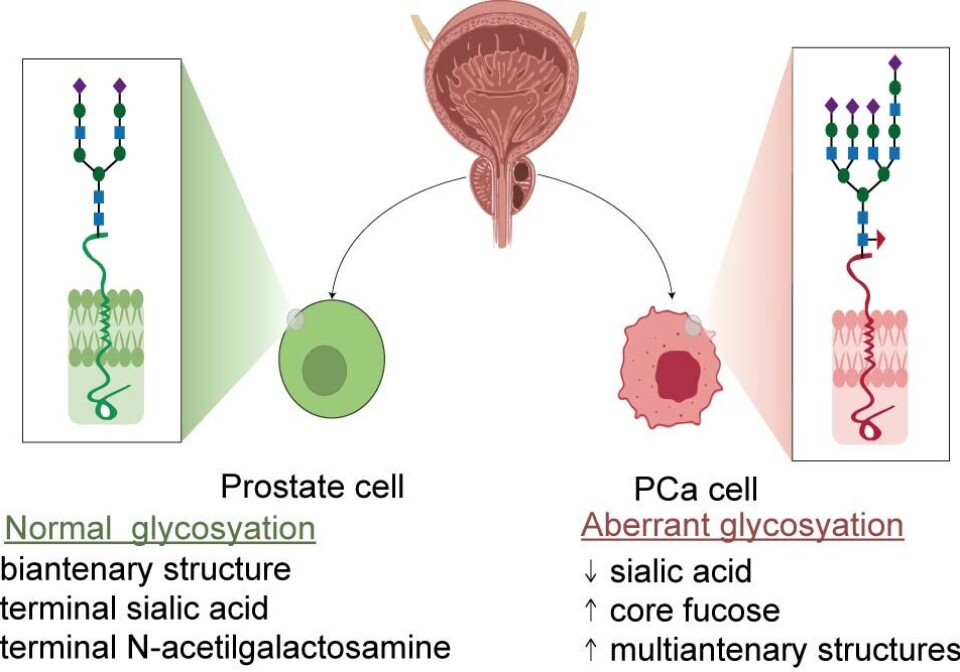
PSA (prostate-specific antigen) isn’t just a protein — it comes with a special sugar coating known as glycosylation.
Cancer leaves behind hidden clues, and one of them is how it changes the sugar coating on proteins.
In healthy men, this sugar structure follows a distinct pattern, mostly made up of neatly branched chains called bi-antennary structures.
But when cancer develops, it scrambles the protein sugar code.
Instead of its usual form, PSA’s sugar structure becomes a mix of different, more complex shapes, with a changed sugar content as well.
We hypothesized that the detecting this broken ‘sugar code’ of PSA could be a more accurate way to detect aggressive types of prostate cancer than simply measuring how much PSA is present in the blood.
The more abnormal the sugar surface, the more aggressive the cancer
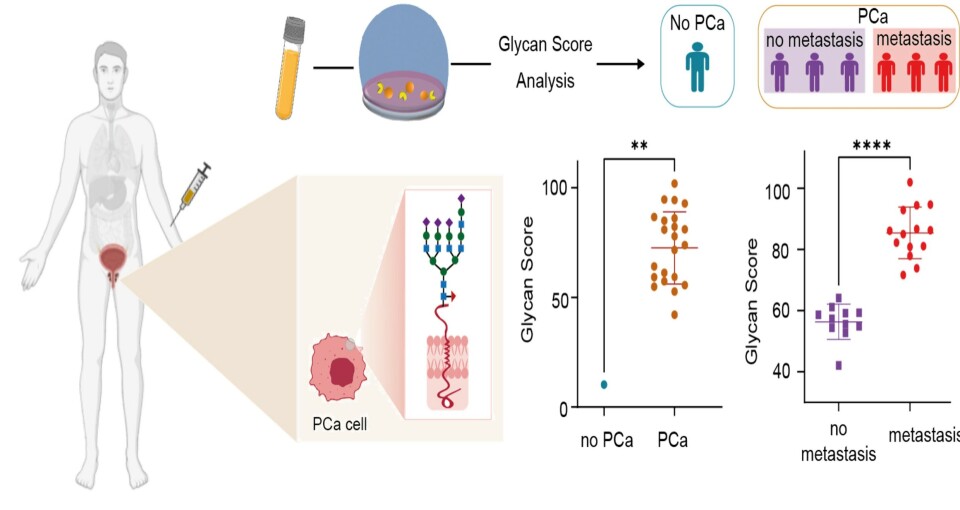
To investigate this idea, we developed a new blood test using ‘DNA aptamers’, which are tiny synthetic molecules that can specifically bind both to PSA and its sugar coating.
Using these aptamers in a special bioelectronic test, we were able to measure how much PSA in a patient’s blood had an abnormal sugar coating. Or with a scientific term: how much PSA was ‘glycosylated’.
We assigned this new way to assess a patient’s prostate cancer status to the so-called ‘Glycan Score’. The scale divides patients into three categories depending on the level of abnormal sugar coating on the PSA-molecules, and we could now use the scale to tell whether a patient has cancer and how aggressive it is:
Healthy individuals: Glycan Score below 30% → Likely cancer-free
Localized (early-stage) prostate cancer: Glycan Score between 39% and 64%
Metastatic (aggressive, spreading) prostate cancer: Glycan Score above 72%
The higher the Glycan Score, the more aggressive the cancer is. This happens because as cancer worsens, it disrupts the natural PSA-protein complexes in the blood, exposing more PSA sugar coating for detection.
The idea to use DNA aptamers to sense PSA sugar coating actually came from Professor Maria Jesus Lobo-Castañon, University of Oviedo, who’s PhD student Ana Diaz-Fernandez designed the original aptamer before joining my research group.
We thought it would be great to try this approach in Denmark for detecting aggressive cancers. It was an absolute discovery that our test can classify metastatic and primary cancers. It took me on year to explain the results, before we were ready to publish them.
Full success in first trial
In our trial of 30 patients, the Glycan Score correctly identified 100 percent of prostate cancer cases — including distinguishing between localized and metastatic cancer.
It even correctly ruled out cancer in one recovered patient.
By contrast, the PSA test (the current standard for population-wide screening) was only 53 percent accurate and could not differentiate between aggressive and less harmful forms of cancer.
If larger clinical trials confirm these findings, the Glycan Score could become a more accurate, reliable tool for doctors and help reduce unnecessary treatments while catching aggressive cancers earlier.
A possible game changer for detecting (and surviving) prostate cancer
With more than 1.4 million estimated cases of prostate cancer worldwide in 2023, the demand for a cheaper, more accurate and user-friendly screening method is high.
For years, the idea of a simple and highly accurate blood test for prostate cancer felt more like science fiction than reality.
Traditional blood tests struggle with precision, which means they can miss serious diseases or raise false alarms. This can lead to unnecessary biopsies—or worse, delayed diagnoses that come too late—ultimately contributing to higher death rates.
But now, the development of the Glycan Score to be used in testing for aggressive prostate cancers might turn that vision into reality, offering a promising new approach for early detection of cancers most difficult to treat.
Still, before these findings can be used in everyday medical practice, larger independent studies with several hundred patients are needed—and we’re eagerly looking forward to them.
These trials are a crucial step toward gaining approval from the FDA and European health authorities.
If fully realized, it enables more accurate large-scale screening programs and provides a more reliable way to monitor treatment responses in advanced cases, bringing us one step closer to detecting and managing prostate cancer is as simple as a routine check-up.
We hope that this will be a major leap forward in the fight against one of the most common cancers in men.





